
- No win. No fee.
- No hidden costs
- 100% risk-free, only pay if you win
- Home >
- Insights >
- Medical Negligence >
- The risks and causes of prescription and medication errors explained
About the Author
Tami Frankel
Medical Negligence Solicitor and Partner - LLB (Hons) University College London
Read more about Tami »Every day, millions of people across the UK trust doctors, nurses and pharmacists to prescribe and administer the medication they need to feel better.
While the vast majority of prescriptions are issued safely, mistakes do happen. Increasingly complex medication regimes, rising prescription volumes and growing workload pressures across the NHS mean medication errors are more common than many people realise.
These errors can result in anything from mild, temporary side effects to permanent, life-changing or life-threatening harm.
This article explains what medication and prescription errors are, how they occur, the risks they pose to patients, and what steps you can take to pursue a prescription or medication negligence claim.
Understanding prescription and medication errors
- What is a medication or prescription error?
- What are the most common types of prescription and medication errors?
- What causes prescription and medication errors?
- What are the potential risks and consequences of medication errors?
- What can I do if I’ve been affected by a medication error?
- Start your medication or prescription claim with Gadsby Wicks
What is a medication or prescription error?
The World Health Organization (WHO) defines a medication error as:
“Any preventable event that may cause or lead to inappropriate medication use or patient harm while the medication is in the control of the healthcare professional, patient or consumer”
Medication errors can be grouped into several key categories:
- Prescribing errors: When GPs fail to prescribe the correct medicine
- Dispensing errors: When pharmacists fail to supply the right medication
- Administration errors: When healthcare professionals administer medication incorrectly
- Monitoring errors: When patients are poorly monitored after taking medication
According to research published by BMJ Quality & Safety, “definitely avoidable” medication errors cause over 1,700 deaths every year, and cost the NHS approximately £98.5 million annually in compensation and legal costs.
Where can medication and prescription errors occur in healthcare?
The medication and prescription errors described above can happen in a wide variety of healthcare settings and situations, both within the NHS and the private health sector. These include (but are not limited to):
- Hospitals and patient treatment areas
- GP surgeries
- Outpatient clinics
- Hospital pharmacies
- Community pharmacies
- Nursing and care homes
- Ambulances and paramedic sites
Research suggests that approximately a third (34%) of harmful medication errors are made when prescribing in primary care settings.
What are the most common types of prescription and medication errors?
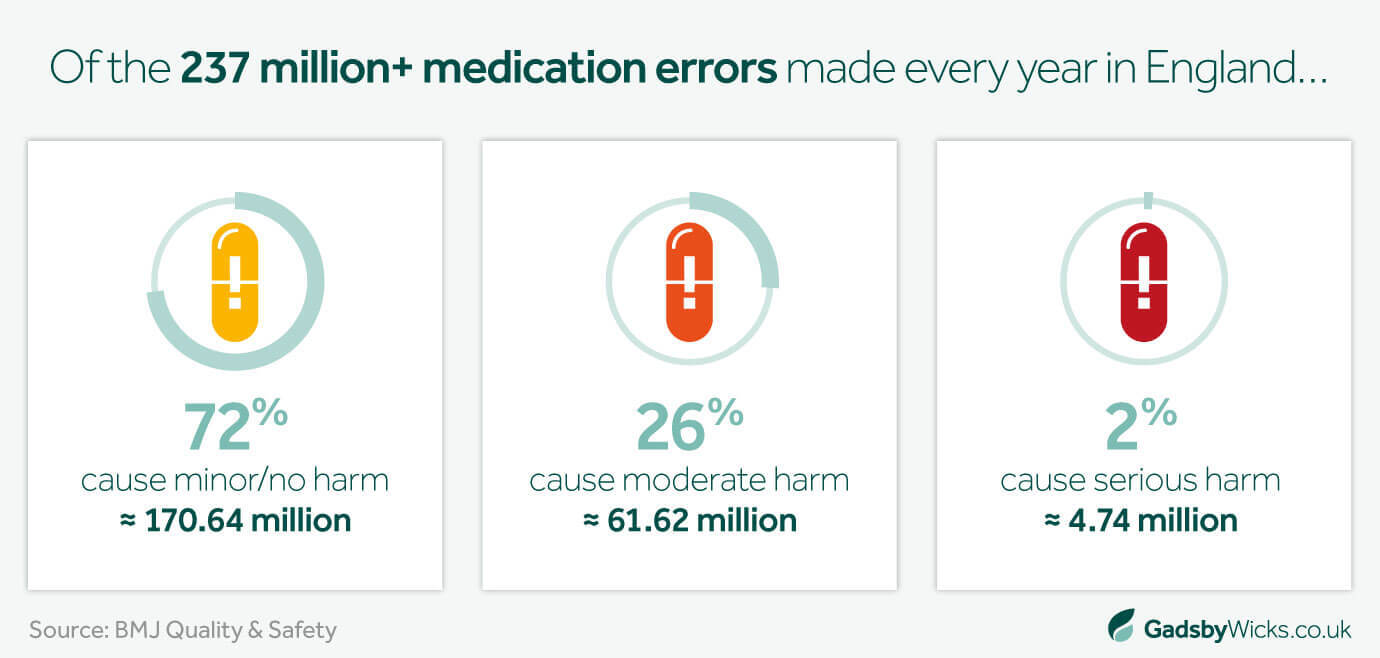
Although rare overall, medication and prescribing errors are widely considered one of the most common forms of medical negligence. It is estimated that there are approximately 237 million medication errors in the NHS every year – with around 30% of these considered harmful to the patients affected (66 million).
While this is just a fraction of the 1.26 billion prescription items issued per year, it is still a significant number. But what forms of prescription and medication errors are the most common?
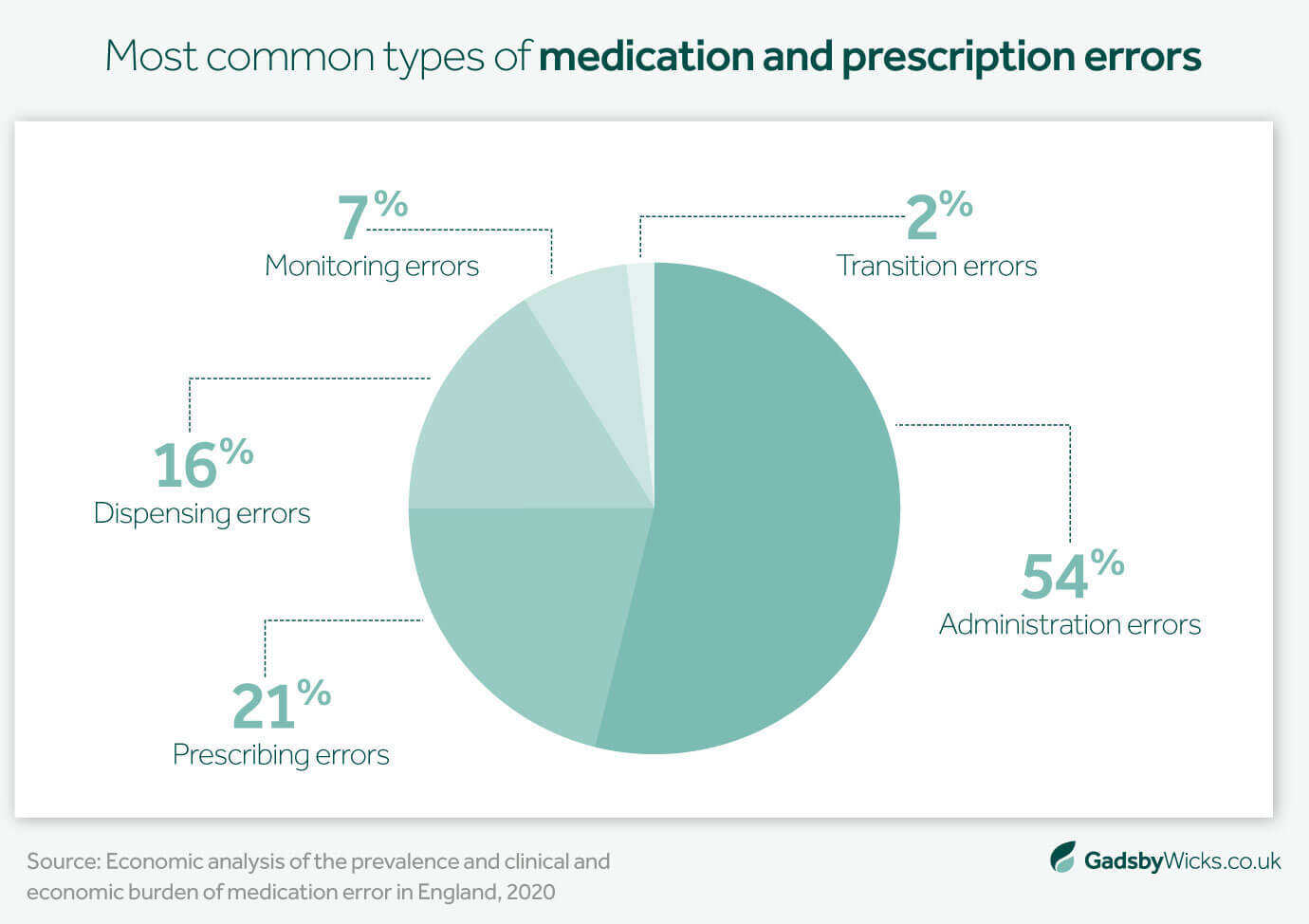
Administration errors
Medication administration errors focus on the actual delivery of a drug to the patient, and whether these lead to preventable harm. Examples include:
- Omission, or not prescribing a medicine that the patient required
- Administering the incorrect dose or strength of medication
- Failure to consider the patient’s allergies or other medications
- Administering medication through the wrong route (injection, IV, oral, etc.)
- Using an unnecessary or inappropriate drug
Prescribing errors
Over a billion prescription items are issued in England each year. While most are prescribed correctly, the sheer volume of NHS prescribing means errors can and do occur.
Examples of these errors include:
- Prescribing the wrong medication or harmful medication for the patient
- Incomplete prescription information, such as dosage, strength, route of administration, or frequency
- Providing too high or too low a dose or strength of medication
- Failure to clearly inform the patient of usage instructions
- Prescribing medication that is not clinically indicated or required
- Repeat prescription errors
These medication errors are especially common in busy NHS hospital wards or care homes.
Dispensing errors
Even if the prescription itself is correct, dispensing or pharmacy errors can be equally harmful for patients. Examples of such mistakes include:
- Dispensing the incorrect drug or medicines
- Not checking prescriptions thoroughly before dispensing
- Labelling errors, resulting in patients receiving the wrong medication or instructions
- Failure to clearly inform the patient of usage instructions
- Supplying patients with the incorrect dosage or strength
Monitoring errors
The final prominent type of medication error in the NHS is monitoring, when healthcare professionals do not adequately review their patients’ progress after receiving medication. Specific situations of this include:
- Follow-up tests or checks after medication is prescribed are either not requested or not acted on (e.g. anticoagulants or lithium)
- Ignoring adverse drug reactions
- Overlooking the patient’s blood levels
- Communication and handover failures
What causes prescription and medication errors?
Now you can recognise common medication errors, how do these mistakes happen? What makes them some of the most frequent forms of medical negligence?
Medication errors rarely have a single cause. They usually arise from a combination of human, system and communication failures, including:
Human factors
First, it is important to acknowledge the pressures on today’s healthcare professionals. Fatigue, high workloads, staff shortages and frequent interruptions can all increase the risk of mistakes.
System and process issues
Beyond individual errors and challenges, wider systematic problems that affect the quality and accuracy of prescriptions include:
- Handover failures can cause patients to receive multiple doses or miss scheduled doses
- Communication failures between services can lead to similar outcomes
- Incorrect timetables or prioritising can mean patients are overlooked for unnecessary lengths of time
Prescription complexity
With new medications introduced and withdrawn each year, the complexity of managing prescriptions is a constant challenge for both GPs and pharmacists.
Polypharmacy (where one person is taking multiple medications at once) makes it difficult to introduce another drug without adverse reactions. Furthermore, many medicines share similar names, colours or packaging.
Finally, complex medication regimes and dosing schedules are also a prevalent cause of prescription errors.
Technology challenges
Technology has played a key role in keeping medication records organised, but they may also be at the root of mistakes.
Overreliance on electronic prescribing and repeat prescription systems can mean doctors and pharmacists do not check prescriptions thoroughly, resulting in avoidable errors.
Patient-related factors
Finally, problems such as unclear patient medication histories, language barriers and self-administration difficulties can also have adverse outcomes for patients.
It is important to note that many safeguards exist across healthcare services to minimise these problems, and medication errors typically occur only when several of the causes above happen simultaneously.
What are the potential risks and consequences of medication errors?
In most circumstances, medication errors have little to no impact on the affected patient. Research suggests that approximately 72% of these instances have minor or zero harmful consequences, while just 2% result in serious harm to the patient.
However, with 237 million medication errors recorded by the NHS annually, that is still up to 4.75 million cases of serious harm per year.
On the milder end of the spectrum, there could be a slight increase in medication side effects, or a temporary worsening of the patient’s symptoms. This may be unpleasant for a while, but likely not enough for a negligence claim.
However, in more serious cases, medication errors can have long-term consequences for the patient affected, such as:
- Intense, frequent side effects
- Allergic reactions
- Adverse drug reactions
- Prolonged illnesses and hospital admission
- Progression of underlying illness or condition
- In rare cases, long-term health problems or life-threatening situations
These repercussions are more likely to be considered suitable grounds for a compensation claim.
What can I do if I’ve been affected by a medication error?
We’ve discussed the various types of medication and prescription errors, how they can be caused and the potential ramifications of these mistakes. But now we come to arguably the most important question – what should you do if you are harmed by a medication error?
Seek medical advice and clarification
Patient safety comes first, so it’s important to contact a GP, pharmacist or another healthcare professional if your symptoms are severe or worsening since you started taking the medication you were prescribed.
They will likely be able to confirm whether the medication, dosage or instructions you received were correct, and advise on your next steps. Early medical input can help to limit the complications of any negligent treatment, and create a clear medical record of what went wrong should you wish to pursue a claim.
Keep medication, packaging and instructions
Retain as much physical evidence related to your medication or prescription as you possibly can, including:
- Remaining tablets or liquids
- Blister packs
- Prescription packaging
- Bottles and labels
- Written prescriptions
- Patient information leaflets
This packaging often contains batch numbers, dosage instructions and dispensing details that may later prove important, both for independent medical reviews and any future complaint or negligence claim.
Do not worry if you can’t gather everything alone – an experienced solicitor can help you gather evidence should you choose to make a claim.
Record the effects of your medication
It can be useful for both your healthcare providers and solicitors to keep a simple timeline or diary, noting when your medication was taken and the symptoms or side effects that followed.
You may also want to take photographs of any consequences of your medication (e.g. rashes, swelling, etc.) to help illustrate how your medication affected you physically.
Of course, nobody expects to be further harmed by the medication that they are given or prescribed, so it is unlikely you would take notes from day one. But as soon as you start to suspect or worry that something is wrong, any first-hand notes can be invaluable when explaining events to your clinicians or lawyers.
Raise concerns with the healthcare provider
Once you believe you were given or prescribed the wrong medicine, you may want to report medication errors to the relevant pharmacy, GP surgery or hospital. Raising concerns with your healthcare providers can help:
- Alert them about system failures, so they can review and fix these
- Provide you with an explanation or answers on what happened to you
- Minimise the chances of the same mistake happening to others in the future
Follow the specific complaints procedures outlined by the individual pharmacy or NHS complaints procedures, which may include reaching out to PALS (The Patient Advice and Liaison Service).
Please be aware that making a complaint, asking questions or raising concerns with your healthcare provider should not affect your future care or treatment.
Reach out for legal advice
Finally, if you believe you suffered preventable harm due to a medication or prescription error, contact a trusted medical negligence solicitor or firm about your legal options.
A capable solicitor will ask about your circumstances and advise on whether you have grounds to make a medication negligence claim based on the three key elements of any claim:
- Did your healthcare provider breach their duty of care to you?
- Did you suffer physically, psychologically and/or financially as a result?
- Were your injuries directly caused by the breach of duty?
Even if you are undecided about making a claim or unsure if you have a case, legal guidance can give you clarity, reassurance and perspective at a difficult time, so please consider it.
Please note that there is typically a three-year time limit from the date you became aware of your injuries to launch a claim. However, the earlier you reach out for legal advice, the better, as it means evidence and people’s recollections will be fresher than if you wait months or years.
Start your medication or prescription claim with Gadsby Wicks
As the only specialist medical negligence team in Essex and East Anglia, we have the experience and expertise needed to determine whether you have a claim and, if so, support you every step of the way to secure the answers, compensation and justice you deserve.
- We have only worked in medical negligence since 1993
- We are strictly “No Win, No Fee” solicitors – you pay nothing unless we win your case
- Our solicitors are accredited by The Law Society, APIL and other reputable bodies
- 96% of our cases are settled before needing to go to court
Secure your financial future and find closure after a medication error – start your claim today by completing our quick questionnaire.
Disclaimer
All content contained within this article is meant for general information only – this should not be treated as a substitute for medical advice from your doctor or another healthcare provider. If you require legal advice specific to your situation, please contact our team directly.
Gadsby Wicks is not liable for any diagnosis made from the content of this article, nor does it endorse any service or external site linked to within the article.
Always consult your GP if you are concerned about your health and wellbeing, or speak to us if you require legal advice.
Related Insights


Can you sue a hospital for medical negligence?



 Back to top
Back to top
