- Home >
- Pressure Sore and Bed Sore Claims
Pressure ulcers and bed sores occur due to unrelieved pressure on the skin or tissue, and are a major risk for anyone with limited mobility. If you or someone you loved developed pressure sores due to inadequate care in a hospital, nursing home or other healthcare setting, you may be entitled to make a negligence claim.
As legal experts with over 30 years of experience in clinical negligence, we understand the tremendous physical and emotional impact pressures sores can have. We work tirelessly to evaluate every aspect of your case and secure the answers, justice and compensation you need to move on from your pain and suffering.

Do you have a pressure sore compensation claim?
Around 95% of pressure sores can be avoided when healthcare professionals adhere to guidelines. If the care they provide falls below standards, there can be serious consequences.
If negligent care led you to develop bed sores in hospital, or someone you love suffered long-term damage from pressure sores at a nursing home, our trusted solicitors are here for you. Through clear advice and diligent investigation, we help you claim compensation that supports your quality of life.

The specialist pressure sore negligence claims solicitors for Essex & East Anglia
Since 1993, Gadsby Wicks has helped hundreds of people affected by pressure sores secure justice – and we can do the same for you.
Working on a strict ‘no win, no fee’ basis, we leave no stone unturned in our investigations, reviewing all evidence and consulting impartial experts to prove your claim – all at zero financial risk to you. With 96% of our claims resolved out of court, trust our attentive, compassionate team to achieve a fair outcome and give you peace of mind.
What does our pressure or bed sore claim process look like?

A free initial consultation
Call us, request a callback or complete our online form and we’ll assess if you have a valid medical negligence claim.

Funding your claim
Discover the ways we can fund your claim without you paying a penny at any stage of the process.

Investigating evidence
We gather medical records, witness statements and more to learn what happened to you and prove your claim.

Instructing independent medical experts
We work with impartial, experienced medical experts to establish whether your injuries were due to substandard medical care.

Valuing your claim
We assess your health and financial losses to accurately estimate how much compensation your claim is worth.

Presenting your case
We contact the Defendants and the Courts on your behalf to set out your allegations and receive a response.

Negotiating a settlement
We work to achieve a fair settlement for you outside the courtroom – this is how 96% of our cases end.

Preparing for Trial
If we must proceed to Trial, we fully prepare you for what to expect so you receive the right result in court.
FAQs about pressure sore and bed sore claims
What is a pressure sore or bed sore?
Pressure sores, sometimes referred to as pressure ulcers, decubitus ulcers or bed sores, occur when a patient experiences unrelieved pressure on their skin and underlying tissue for an extended period.
These issues typically appear in parts of the body where a bone is close to the skin, such as the shoulders, elbows, heels, lower back and bottom.
There are four grades of pressure sores, with a Grade 1 pressure sore being the least harmful and a Grade 4 pressure sore presenting the greatest risk:
- Grade 1: Skin discolours and can begin to feel warm, spongy or hard, causing a degree of pain or itchiness in the affected area
- Grade 2: Partial skin loss occurs, presenting as an open wound or blister
- Grade 3: A deeper wound forms that reaches lower levels of the skin, presenting like a crater on the skin
- Grade 4: A very deep wound forms that may reach muscle or bone, potentially leading to extensive necrosis to the underlying tissue
While the majority of bed sores are identified at an early grade and treated without serious consequences, a Grade 3 or 4 pressure sore can have dangerous complications. This can often be the basis for making medical negligence claims.
Who is at risk of developing pressure sores?
Pressure sores or bed sores can affect anybody. According to the NHS, 1 in 20 people who are admitted to hospital with a sudden illness will go on to develop a pressure sore.
The greatest risk factor for developing pressure sores is a sustained period of immobility. Older people in care homes are also generally at greater risk of developing sores.
NICE guidelines on treating patients with mobility problems, or who cannot move following surgery, help prevent these sores from forming. These guidelines include frequently turning patients, providing appropriate bedding and conducting at least one weekly thorough check for warning signs.
View our National and Essex Medical Negligence Statistics post for more industry insight.
What complications can result from a pressure sore?
Although uncomfortable, a Grade 1 pressure sore is not very dangerous. However, these injuries can carry a great risk if they become an open wound and go untreated for extended periods. In rare cases, severe pressure sores can be life-threatening.
As pressure sores typically develop on areas of the body that are close to bones, osteomyelitis (bone infection) is a major concern for Grade 3 and Grade 4 pressure ulcers. These can be extremely dangerous, depending on the nature of the infection, and may require bones or joints to be surgically removed.
Septicaemia is another concern. If an infection in a pressure sore can spread through the bloodstream into other organs, this can result in a significant drop in blood pressure, known as septic shock, which can unfortunately be fatal.
Other serious consequences of a pressure sore include:
- Cellulitis, which is an infection that spreads from the ulcer into a deeper layer of skin
- Necrotising fasciitis, also known as “flesh-eating bacteria”, which is a serious skin infection that can lead to the rapid death of tissue around the wound
- Gas gangrene – a rare infection where the pressure ulcer is infected with clostridium, which releases dangerous toxins that can cause severe pain and swelling
- Damage to the heels that can make walking painful and challenging
- Development of extensive necrotic tissue, which may require amputation to remove the threat of potentially fatal infections
How can negligent care lead to pressure sores?
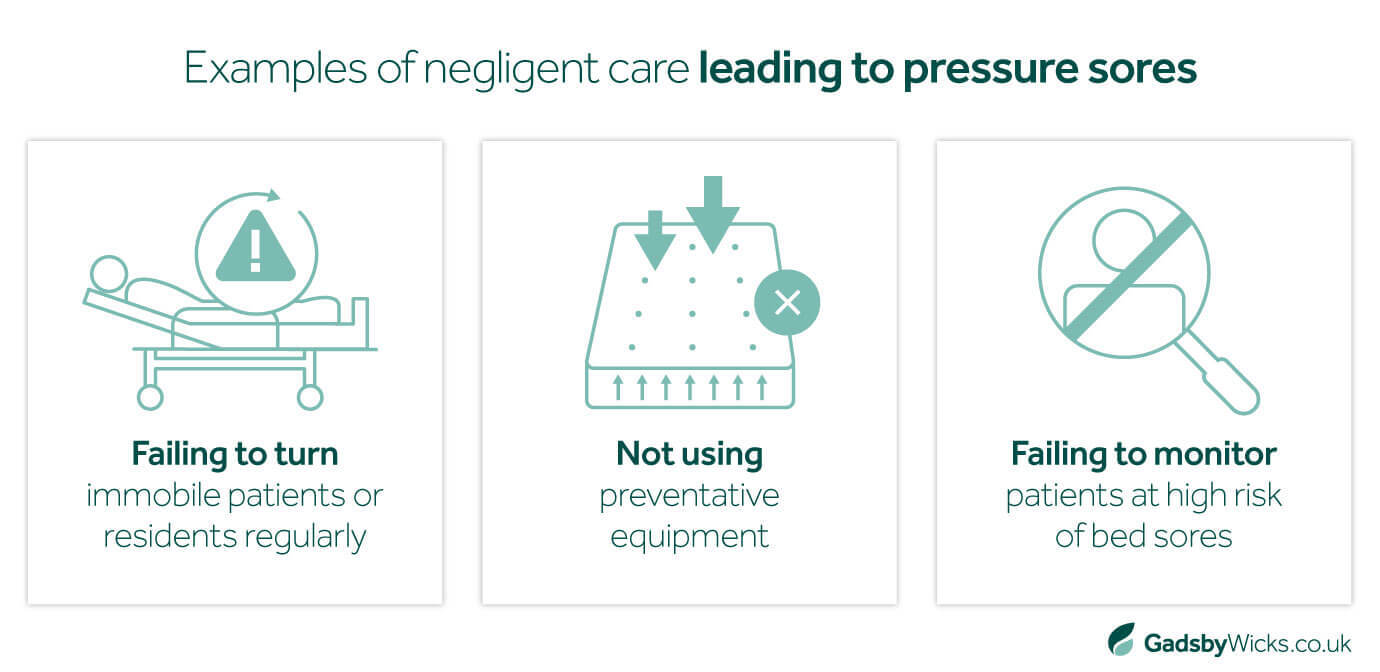
When best practices are followed, medical professionals can prevent pressure sores from developing in 95% of cases. Sadly, these guidelines are not always adhered to. As a result, the failure to prevent pressure sores is the most common basis for this type of claim. In practice, this could mean:
- Nurses or other healthcare professionals fail to turn an immobile patient or resident regularly
- Preventative equipment, such as pressure-relieving mattresses, were not issued where required
- Patients thought to be at high risk of developing pressure ulcers did not receive regular monitoring
As well as failing to prevent pressure sores, issues monitoring an existing ulcer or avoidable delays in treating an injury can also be grounds for a negligence claim.
If you are seeking legal advice for your pressure sore claim, get in touch with our experienced solicitors today, or find out if you have a valid claim online.
How do you prove medical negligence occurred in a pressure sore claim?
To prove negligence in a pressure sore claim, three key elements must be satisfied:
- There was a breach in your healthcare provider’s duty of care
- You suffered pain, injury, financial loss or damage
- Your suffering was directly caused by your healthcare provider’s breach of duty
All medical negligence claims are determined on the Balance of Probabilities. This means that you must prove that it is more likely that your injuries were caused by the Defendant’s negligence than not.
As specialist medical negligence solicitors, we do this by gathering and assessing all available evidence connected to your claim, including:
- Medical records
- Personal statements
- Witness statements
- Photographs
We will also consult with impartial medical experts throughout our investigation. Their experience is crucial in understanding what happened to you, determining whether or not your healthcare provider breached their duty of care, and quantifying the amount of compensation you can pursue.
To learn more about how we investigate and resolve medical negligence cases of this nature, explore our claims process.
Can I sue a care home for pressure sores?
Yes. If you believe you or a loved one's pressure sores were caused or worsened due to inadequate treatment from care home staff, you can pursue a negligence claim against the care or nursing home.
Contact our expert pressure sore and bed sore claims solicitors
If you or someone you care about developed severe pressure sores due to negligent medical treatment, speak to our team about your options. We are here to listen and advise you on your next steps.

Lexcel accredited medical negligence claims solicitors
We are proud to be a Lexcel-accredited practice. The accreditation is a mark of quality and comes directly from the Law Society.
A recent assessment described us as a “Centre of Excellence” and we continue to operate to the highest standards across all main areas of our field. These include client care, case management, financial management, structure and strategy, people management, risk management, information management and file management.